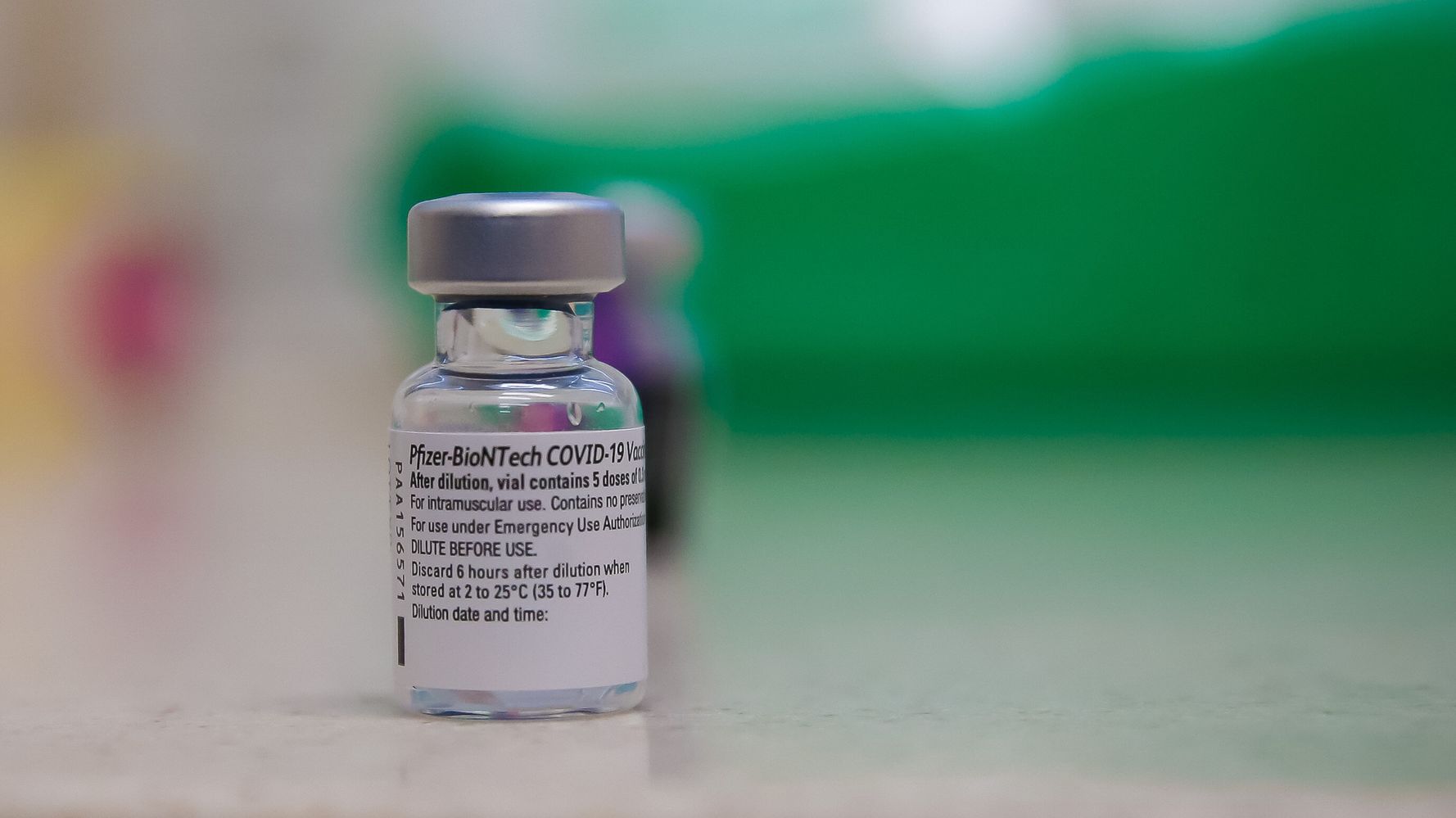
The arrival of coronavirus vaccines from Pfizer and Moderna has offered a much-needed dose of optimism in an otherwise grueling pandemic. But many people have questions after reports of some instances of allergic reactions to the Pfizer/BioNTech vaccine, which was granted emergency authorization use by the U.S. Food and Drug Administration earlier this month.
Some people who were administered the vaccine reportedly experienced anaphylaxis or a less severe allergic reaction, which was not seen in the vaccine trials.
The FDA is investigating the cases of allergic reactions, and the Centers for Disease Control and Prevention has said that anyone who had a severe reaction (which is defined as needing the medication epinephrine or treatment in a hospital) should not get the second dose of the vaccine.
So, does this mean we be super concerned? Here’s everything you need to know right now about the vaccine and any allergic reactions that may come up:
The percentage of people who have actually experienced an allergic reaction to the Pfizer vaccine is low.
The FDA is looking into about five cases of allergic reactions reported in people who received the first dose of Pfizer’s COVID vaccine. The cases occurred in several parts of the country.
This is concerning, yes. However, when you compare the number of these cases to the total number of people vaccinated so far ― roughly at least 128,000, or even more when you count the people who participated in the trials ― the percentage of people experiencing this issue is pretty small.
“With large numbers of people being vaccinated, reports of allergic reactions are very rare and have been easily treated with resolution,” Daniel Griffin, chief of infectious disease at ProHEALTH Care and national process expert for Optum Vaccine Administration, told HuffPost.
Most people, including those with specific allergies, shouldn’t be too stressed out about the vaccine right now, Griffin said.
“Only people with a severe reaction to a prior vaccination should be concerned, and we recommend they discuss this with a doctor prior to vaccination,” he said. “People with other allergies, such as to food, pollen or even antibiotics, need not worry.”
It’s not clear if Moderna’s vaccine will cause the same issue.
Kavita Patel, HuffPost medical contributor and a practicing internal medicine physician in Washington, D.C., said in a recent HuffPost Q&A that Moderna’s data from the vaccine trials submitted to the FDA showed no severe allergic reactions.
That said, this isn’t a guarantee that no one will experience a reaction if they get the Moderna vaccine ― which was also just granted emergency authorization use by the FDA ― rather than the Pfizer vaccine. Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research, said in a recent press conference that a chemical used in both vaccines, called polyethylene glycol, could be what’s causing the reactions, Reuters reported.
Griffin said experts will know more once a greater number of people are vaccinated. As of now, the FDA is advising that the Moderna vaccine should not be given to people with a known history of severe allergic reactions to any components of the immunization.
Most vaccines cause allergic reactions in some people.
Allergic reactions like this aren’t unique to the COVID-19 vaccines. Overall, this news shouldn’t cause extreme vaccine hesitancy or alarm for the general public.
“Most vaccines cause allergic reactions in a few people, so there is nothing new with the COVID vaccines,” Griffin said. “These reactions appear rare, and may be even less common with the COVID vaccines than other vaccines.”
If you’ve experienced an allergic reaction to a vaccine in the past, talk to your doctor before you get a COVID vaccine.
We still have a long way to go before a COVID-19 vaccine is available to most people, so this won’t really even be an issue for quite some time. When it’s your turn to get the shots, talk to your doctor about your specific case, including your known allergies and any history you might have of vaccine reactions.
“If you have had a serious reaction to prior vaccines, you might not be able to receive the vaccine, or at a minimum might need to discuss the reaction with your provider and determine if it’s still reasonable to get it,” Patel said.
Griffin said some patients with a history of vaccine reactions “may be advised to take an antihistamine such as Benadryl 30 minutes prior to vaccination.” Your physician may also monitor you for an additional 30 minutes after you get your dose, to make sure you’re OK.
And remember, there are other ways to protect yourself from COVID-19 in the meantime: Wear a mask, wash your hands and keep your distance from people who aren’t in your household. We’ll likely have to continue these measures for some time anyway, even with an available vaccine.
Experts are still learning about COVID-19. The information in this story is what was known or available as of publication, but guidance can change as scientists discover more about the virus. Please check the Centers for Disease Control and Prevention for the most up-to-date recommendations.